My thoughts on breathing...
A bit more information as it occurs to me about how breathing impacts your health and well-being. If you have questions or want me to address a particular topic, please don't hesitate to contact me!
 Time for another installment of "What's breathing got to do with it?" This time we are talking about sleep, because, as it turns out, breathing and sleep are pretty intricately related. Today we will look at a few ways that poor breathing patterns might be impacting your quality of sleep. Getting to sleep Do you climb into bed each night, only to lie there staring at the ceiling, wondering when sleep will come? A lot of patients that I see report having difficulty falling asleep. These patients also tend to have a more stimulating breathing pattern: rapid and dominated by upper chest movement. This type of breathing tends to keep the body in a hyper-aroused state - it's ready for anything, anytime. Indeed, research has shown that patients with insomnia have increased brain activity, abnormal hormone secretion, elevated heart rate and sympathetic nervous system arousal when they do sleep. It's as if their bodies don't know how to turn off. This is where breathing retraining comes in. Learning how to engage in a slower, more effortless breathing pattern, can help to activate our parasympathetic nervous system. This the "rest and digest" part of our autonomic (automatic) nervous system, and helps to put the brakes on the flight or fight side. Those of us who try to cram as many things into the day as possible, running from one activity to the next, dealing with stressful work situations, spouses, kids, etc may not remember what it feels like to turn off, tune out and relax. Learning how to let go as well as using mindfulness to help deactivate the stress response is key to getting the body better prepared for transitioning to sleep. I've had many clients report that they ended up falling asleep practicing finding calm- and that wasn't even the intended goal! Breathing During Sleep During normal sleep stages, several changes occur to our breathing. As we transition into sleep, there is a decrease in signals to the muscles of the chest and upper airways. This results in increased resistance in the upper airways and less activation of the chest muscles. During the next transition into REM sleep, all of the skeletal muscles of the body become atonic - meaning they relax nearly completely. The theory behind this being that we do not then act out our dreams. During this time, breathing is critically dependent on the function of the diaphragm, as it will often have an increase in activity. For most individuals, these changes to breathing patterns at night do not pose a problem. However, for anyone that has altered breathing patterns due to diaphragm weakness, this can lead to sleep disorders. Diaphragm weakness is seen in a number of situations:
Treatment for Sleep Disordered Breathing The gold standard for addressing sleep apnea is continuous positive airway pressure - or CPAP. Essentially a machine will deliver a constant stream of air through the mouth or nose at night to ensure that the airways do not collapse and cause a stoppage in breathing. In addition, lifestyle changes such as weight loss and sleep hygiene are encouraged. What is also showing some promise in the treatment of sleep apnea, is inspiratory muscle training (IMT). IMT strengthens the diaphragm, and studies are showing that IMT can decrease snoring, improve sleep quality and decrease blood pressure issues related to sleep apnea. IMT is non-invasive, inexpensive and relatively easy to perform and should be considered to help treat sleep apnea. In addition to strengthening the diaphragm, there has also been some interesting results using didgeridoo playing as a way to tone the muscles of the upper airways. One ear, nose and throat doctor in the UK advocates the use of these exercises to help tone the throat muscles to help reduce snoring. Another study suggests that singing might just do the same! If you are concerned about your sleep quality, feel free to drop us a line to discuss what kind of treatment options we have here at Breathe Well Physio. We can help you turn off the fight or flight response to help you transition to sleep if you struggle to fall asleep. We can also get you started with an IMT program to strengthen your diaphragm to get you through all sleep phases. And if the problem is your upper airway function, we even offer voice exercises from a professional voice teacher to help tone those muscles to reduce snoring and sleep disruptions!
0 Comments
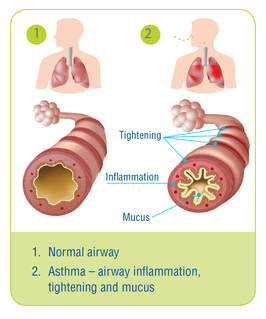 Image from www.lung.ca Image from www.lung.ca Well I suppose that seems like an obvious title. Of course breathing has everything to do with asthma, but today we are going to look at it from a slightly different perspective. We'll think outside the lung so to speak, although first we need to just quickly review what asthma is and why it makes breathing difficult. What is Asthma? Asthma is classified as a chronic disease that affects the airways or breathing tubes. With asthma, the airways tend to be more sensitive to things like air pollution, cold, viruses and sometimes exercise. Airways become inflamed and swollen, and the muscles around them also contract, making it harder to breathe - think of trying to drink a thick milkshake through a very tiny straw instead of a fat one. Symptoms of asthma include shortness of breath, wheezing (noisy breathing), coughing and tightness in the chest. When triggered, the increased struggle to breathe can lead to feelings of anxiety and panic - which makes sense, since for our brain, breathing is the number one thing it tries to preserve on a daily basis. Why Think Outside the Lung? So the good news about asthma, is that it responds quite well to medications and therfore is labelled as "reversible." This does not mean that medications cure asthma, simply that they can help control the inflammation and make breathing easier. However for some people, despite having optimal medication therapy, symptoms of breathlessness persist. And in these instances, we need to think outside the lung to understand why. When breathing is difficult - whether due to asthma, or maybe heavy exercise or sometimes even from a really bad cold - our body calls upon our helper, or accessory, muscles of breathing. These muscles are located in the chest, neck and shoulder region and help to lift up the ribs and breastbone to allow for more enter the lungs. At this point, we may also switch to mouth breathing as it offers up less resistance to breathing. You can try this on yourself to see: put one hand on your chest and one on your belly and breathe normally through your nose. Now open your mouth and take a slightly bigger breath. You will notice that your breathing has less resistance and your chest moves more than with your mouth closed. When breathing is more laboured, this mouth-chest breathing pattern is a good response to have. The problem arises when this emergency response breathing pattern becomes the new normal. This can happen in people with asthma. Studies (see references below) have shown that breathing dysfunction is common in persons with asthma, and that sub-optimal breathing patterns are associated with decreased perceived asthma control. The reasons behind changing breathing patterns are many, but the important point is that most dysfunctional breathing patterns are learned. Here is an example of how the body learns: let's say Mary has asthma. When Mary's asthma is triggered, she feels anxious and short of breath. When she takes her medication, her symptoms are relieved. However, Mary goes to work, she has a manager that she doesn't get along with. Often, interactions with her manager leave Mary feeling quite anxious and short of breath. When she feels this way, Mary takes her asthma medication because she feels like it could be her asthma. Only the medications don't seem to help. She returns to her doctor for more testing because her asthma symptoms are worsening. The testing shows her lungs are not any worse, despite her increase in breathlessness. This is a common scenario in my practice. What has happened is that Mary's stress and anxiety from work triggers a similar response to asthma. Poor breathing patterns can often mimic asthma symptoms, yet because the problem is not airway inflammation, medications don't often help. Sometimes, being anxious and changing your breathing pattern (generally, anxiety causes a faster, shallow breathing pattern) may actually trigger asthma too, so it can become a bit confusing. How Physiotherapy Can Help So what is someone like Mary to do, if the testing shows her lungs are not any worse, yet her symptoms are? Accessing treatment by a physiotherapist trained in treating breathing disorders may be a step in the right direction. Here at Breathe Well Physio, we become "breathing detectives" to find out what is causing the symptoms. We look at breathing patterns and breathing chemistry, we factor in things like stress, anxiety and sleep and we also look at how you move (you'd be surprised at how many people come through our doors that hold their breath every time they move!). There is plenty of evidence to support the use of breathing retraining as a way to improve asthma control (again, see the references listed below). Learning optimal breathing strategies and incorporating them into everyday functional activities is essential in helping to control asthma. For Mary, a big component would be recognizing the difference between asthma and stress-related breathing dysfuntion. We may not be able to do anything about Mary's manager, but we can teach Mary to recognize her physical symptoms and use strategies to help settle them. I must point out at this point, breathing retraining is not meant as a "cure" for asthma - and I would advise anyone with asthma to be very wary of any product or method that claims to cure asthma. Breathing retraining is an adjunct to medical therapy and is not a replacement. It is also very important, given that statistics show nearly 30% of asthma diagnoses are actually misdiagnosed, that if you have been told you have asthma, be sure this is confirmed with appropriate lung testing. Simply being out of breath when exposed to environmental allergens or exercise is not enough to confirm asthma. If you are wondering if you can get better control of your asthma or have concerns about your breathing, be sure to check in with us here at Breathe Well Physio and we would be happy to discuss it with you. Until next time...breathe well, move well ...BE WELL! References: Mike Thomas, R K McKinley, Elaine Freeman, Chris Foy. Prevalence of dysfunctional breathing in patients treated for asthma in primary care: cross sectional survey. BMJ VOLUME 322 5 MAY 2001 bmj.com Jane Upton et al. Correlation between Perceived Asthma Control and Thoraco-Abdominal Asynchrony in Primary Care Patients Diagnosed with Asthma. Journal of Asthma, 2012; 49(8): 822–829 Eirini Grammatopoulou et al. The Effect of Physiotherapy-Based Breathing Retraining on Asthma Control. Journal of Asthma, 48:593–601, 2011 Elizabeth A Holloway, Robert J West. Integrated breathing and relaxation training (the Papworth method) for adults with asthma in primary care: a randomised controlled trial. Thorax 2007;62:1039–1042. doi: 10.1136/thx.2006.076430 |
AuthorI'm a physiotherapist who is passionate about educating anyone and everyone about the impact breathing has on our health. Archives
November 2020
Categories |